Understanding Your Options
Pelvic organ prolapse is caused by a weakening of the normal support provided by muscles and tissues of the pelvic floor. The main cause of pelvic organ prolapse is pregnancy and childbirth, especially vaginal childbirth. Other factors include prior pelvic surgery, menopause, and aging. Activities or conditions that increase pressure in the abdomen, such as a long-lasting cough, obesity, or straining with bowel movements due to constipation, can play a role in pelvic organ prolapse. Prolapse also runs in families.
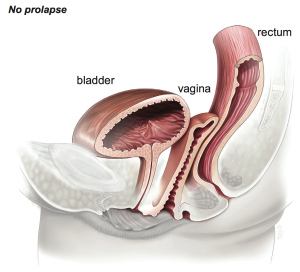
Pelvic organ prolapse usually involves more than one organ. The organs that can be affected include the following:
- Uterus
- Top of the vagina in women who have had a hysterectomy (the vaginal vault)
- Front (anterior) wall of the vagina (usually with the bladder, which is called a cystocele)
- Back (posterior) wall of the vagina (usually with the rectum, which is called a rectocele)
- The pouch between the rectum and back wall of the uterus (usually with a part of the small intestine, which is called an enterocele)
In severe prolapse, the woman can see or feel a bulge of tissue at or past the vaginal opening. Most women have mild prolapse – the organs drop down only slightly and do not protrude from the opening of the vagina – and do not have any signs or symptoms. Some women with mild prolapse and women with severe prolapse do have symptoms, which can include the following:
- Feeling of fullness or heaviness in the pelvic region
- Pulling or aching feeling in the lower abdomen or pelvis
- Painful or uncomfortable sex
- Difficulty urinating or having a bowel movement
If you do not have any symptoms or if your symptoms are mild, you do not need any special follow-up or treatment beyond having regular checkups. If you have symptoms, prolapse may be treated with or without surgery.
Nonsurgical treatment options usually are tried first. Often the first nonsurgical option tried is a pessary. This device is inserted into the vagina to support the pelvic organs. There are many types of pessaries available. A health care provider can help you find the right pessary that fits comfortably. Targeting specific symptoms may be another option. For example, bowel problems can be addressed with behavioral changes, dietary changes (such as adding more fiber to the diet), and stool softeners. Kegel exercises may be recommended in addition to symptom-related treatment to help strengthen the pelvic floor. Weight loss can decrease pressure in the abdomen and help improve overall health.
When symptoms are severe and disrupt a patient’s life and if nonsurgical treatment options have not helped, surgery is an option. The following factors should be considered when deciding whether to have surgery: age, child-bearing plans and health conditions.
There is no guarantee that any treatment—including pelvic prolapse surgery—will relieve all of your symptoms. Pelvic prolapse of the same site can come back after surgery. Prolapse also can occur at a new site after surgery. Depending on whether you have symptoms, additional treatment with nonsurgical options, such as a pessary, or surgery may be needed.
Laparoscopic (or Robotic-assisted) Uterosacral Ligament Suspension
A uterosacral ligament suspension involves suturing the uterosacral ligament to the top portion of the vagina. This procedure is normally performed by placing two sutures through each uterosacral ligament and then through the cuff or apex of the vagina. The suture is tied to support the cuff or apex to the uterosacral ligaments.
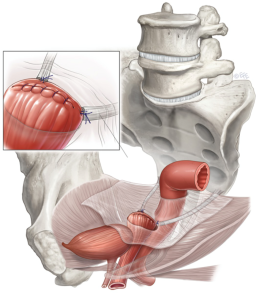 By performing the uterosacral ligament suspension minimally invasively, the vagina is restored to its anatomic position in a minimally invasive manner. Most surgeons perform this procedure through a large incision or through the vagina. A large abdominal incision (laparotomy) will contribute to a longer recovery time. If performed vaginally there is often difficulty identifying the uterosacral ligaments appropriately. The laparoscopic approach allows Dr. Rebeles to define the ligaments readily and also identify key anatomic structures.
By performing the uterosacral ligament suspension minimally invasively, the vagina is restored to its anatomic position in a minimally invasive manner. Most surgeons perform this procedure through a large incision or through the vagina. A large abdominal incision (laparotomy) will contribute to a longer recovery time. If performed vaginally there is often difficulty identifying the uterosacral ligaments appropriately. The laparoscopic approach allows Dr. Rebeles to define the ligaments readily and also identify key anatomic structures.
(Please also see: Robotic-Assisted Prolapse Repair under Robotic Surgery )
Laparoscopic (or Robotic-Assisted) Sacrocolpopexy
 This is a procedure to correct prolapse of the vaginal vault (top of the vagina) in women who have had a previous hysterectomy. The operation is designed to restore the vagina to its normal position and function.
This is a procedure to correct prolapse of the vaginal vault (top of the vagina) in women who have had a previous hysterectomy. The operation is designed to restore the vagina to its normal position and function.
Sacrocolpopexy is traditionally performed through an abdominal incision which requires a prolonged recovery time. Few surgeons are trained to perform this procedure via a minimally invasive approach.
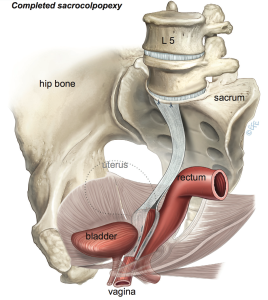 The vagina is first freed from the bladder at the front and from the rectum at the back. A graft made of permanent synthetic mesh is used to support the front and the back surfaces of the vagina. The mesh is then attached to a ligament overlying the sacrum (tail bone) as shown. The mesh is then covered by a layer of tissue called the peritoneum which lines the abdominal cavity; this prevents the bowel from getting stuck to the mesh.
The vagina is first freed from the bladder at the front and from the rectum at the back. A graft made of permanent synthetic mesh is used to support the front and the back surfaces of the vagina. The mesh is then attached to a ligament overlying the sacrum (tail bone) as shown. The mesh is then covered by a layer of tissue called the peritoneum which lines the abdominal cavity; this prevents the bowel from getting stuck to the mesh.
(Please also see: Robotic-Assisted Prolapse Repair under Robotic Surgery )